Until recently, medical school curricula had been largely unchanged since Abraham Flexner outlined the Structure/ Process format of medical education in 1910. For most of the past century, students were trained in a binary system: two years of the basic sciences (anatomy and physiology, pathology and bio- chemistry) followed by two years of clinical training. That was fine for a world in which doctors learned, essentially, a trade that was:
- hyper-rational
- focused on sickness and acute care
- targeted at individuals as opposed to communities
- practiced (more or less unchanged) for decades.
But with the explosion of information and technology, the repositioning of the doctor from kingpin to team member, and the recognition that doctors are integral players in an enormously complex system, medical schools are being forced to adapt.
With input from organized medicine (the American Medical Association, the Association of American Medical Colleges, others) curricula have begun to change. Some schools have responded to the call for doctors to be more familiar with the rapidly evolving healthcare environment by adding courses in health systems science, medical economics and quality/safety measures. Competency-based education is gaining momentum. Recognizing that the information learned in medical school becomes rapidly out-of-date, some institutions have incorporated adaptive learning (learning how to learn) into their core training.

EVOLVING MEDICAL EDUCATION
We are in the middle of a paradigm shift in medical education. While there is yet no dominant, overarching philosophy like Flexner’s, competency-based education may well crystallize into its replacement. Medical schools will be labs for experimentation. Gradually, new best practices will emerge. In the meantime, look for the following changes to play out over the next ten years.
COMPETENCY-BASED EDUCATION
-
COMPONENTS
Identifying outcomes
Defining performance levels
Creating a framework for evaluation
Continually assessing programs
-
DOMAINS
Patient care
Knowledge for practice Practice-based learning
Interpersonal/communication skills
Professionalism
Systems-based practice Interprofessional collaboration Personal & professional development
MORE COMPETENCY-BASED CURRICULA, MORE ADAPTIVE LEARNING ELEMENTS
One early example: Stanford and Khan Academy are piloting a program for self-directed medical coursework.
MIXED REALITY
Virtual reality and augmented reality will continue to make inroads into medical education. VR systems allow students to experience surgery more intimately (and at scale) than trying to see over a surgeon’s shoulder, and the addition of haptic feedback to surgical VR training modules will enable students to train in hands-on simulated environments. VR is already being used to enhance empa- thy, for example, by letting students experience life as an 80-year-old man with hearing and vision problems. VR/ AR anatomy will take students inside the body and give them exposure to the dynamics of disease progression, physiological changes and the effects of interventions.
VR currently used in medical education:
- CPR training for medical providers and patients (Next Galaxy and Miami Children’s Health System developing modules to teach CPR)
- Surgery instruction from a rst-person point of view (The Virtual Surgeon by Medical Realities)
- Trauma simulations (Royal College of Surgeons in Ireland)
- Empathy training (Embodied Labs and the University of Illinois, Chicago)
- Anatomy (Unimersiv)
The impact of VR and AR will be felt beyond medical education as they become more integrated into practice. For example, surgeons already use VR to plan and practice surgery before ever cutting the patient.
MD+IT
Technology won’t just change how doctors learn, but what they learn. In addition to EHRs, 70% of physicians used electronic resources during patient consultation hours in 2016, up from 47% in 2014. Medical school curricula and postgraduate training will need to prepare doctors to be more effective using digital tools like messaging, video chat, AR and VR. More students will be offered classes in interpreting AI-generated data and making individual treatment recommendations for specific patients (like a course currently being offered by Harvard-MIT).
MORE THREE-YEAR MEDICAL DEGREES
Currently, there are nine medical schools that offer three-year degrees. More are planned. Though some programs track students into primary care, others offer access to specialty training. First-mover schools will have a competitive advantage for applicants who know the specialty they’ll pursue, want to open time for additional training and/or want to reduce their debt burden.
By compressing core medical curricula (basic science, organ system, core clinical rotations) into 2.5–3 years, medical schools will allow students to gain additional training in nonclinical disciplines—innovation and translational medicine, healthcare policy and organizational science, data science and genomics. For example, Mayo Clinic School of Medicine in Arizona will enroll its first class in 2017, and all students will be awarded a certificate in science of healthcare delivery in addition to their MD. USC offers an accelerated four-year MD-MPH degree.
MORE COMBINED DEGREES, MD + OTHER
MD-MS, MD-MPH and MD-MBA programs will proliferate. There are currently 65 MD-MBA joint-degree programs, more than double the number in 2000. Such ancillary training will also move into post-graduate (residency) training, where elective time may be dedicated to more formal education (graduate degrees, for example).
TEAM PLAYERS, NOT SOLOISTS
Recognizing that medical care delivery is becoming more team-based, schools will shift their focus in the types of applicants they admit. There will be less emphasis on individuality, more on collaborative potential. Tools to evaluate candidates’ soft skills (like the McMaster Multiple Mini Interview) have been adopted by many schools internationally and will gain traction in the United States.
MED SCHOOL 2.0: BALANCED AND FLEXIBLE
Medical school applicants’ attitudes toward the profession will be “push- pull,” both responding to changes in the job market and forcing changes. Expectations of autonomy will adjust downward, both structurally (working as an employee instead of as a practice owner, for example) and in practice (following protocols and AI-generated diagnoses and treatment plans). Conversely, the demand for work-life balance will intensify. More schools will train students for practice in their own systems, e.g., Kaiser’s new school of medicine, opening in 2019.
INTEREST IN PURSUING A MEDICAL DEGREE WILL REMAIN HIGH
Currently, less than 40% of medical school applicants actually gain admission to medical school. Even a significant falloff in applications will still result in most (if not all) medical schools filling their classes.
By 2025, the Association of American Medical Colleges predicts that there will be a shortage of up to 95,900 doctors (35,600 primary care MDs and 60,300 specialists) despite a 25% increase in the number of graduating medical students 2002–2016. The major drivers are an aging population and the Affordable Care Act, which brought millions of new patients into the healthcare system.
However, the rise of nonphysician providers and the influence of technology will be profound, and we predict that the perceived doctor shortage will become a doctor glut for some specialties.
RADIOLOGY IS THE CANARY IN THE COAL MINE
A radiologist’s job is to analyze data and look for patterns and deviations from patterns, things that computers and AI do well (and computers don’t need to sleep). AI will pre-read images—highlighting areas of concern and offering possible diagnoses, noting incidental findings—cutting down on read times and, despite an overall increase in medical imaging, reduce the total amount of work for radiologists. Technological dislocation and imbalanced labor supply- demand mean that the disruption of radiology is in full swing:
-
01Enlitic’s deep learning radiology platform performed 50% better than human radiologists in classifying malignancies and had a false-negative rate of 0%.
-
02IBM’s acquisition of Merge Healthcare gave Watson a 30-billion-image dataset from which to learn radiology.
-
03Radiology as a specialty is becoming less attractive:
- » 10% drop in residency slots 2013–2017
- » 30% of radiology residency programs unfilled in 2016
- » Starting salary decrease from $450,000 to $300,000.
- » Competition for radiology residencies—one of the most in demand as recently as 2009—was by 2014 less than that for pediatrics, historically one of the less competitive.
Aspects of endocrinology, anesthesia, intensive care and radiology are primarily data driven, therefore they would be some of the early areas ripe for the use of AI, ML and automation.
Sumbul Desai
Apple and Stanford University
PATHOLOGY HAS A SIMILAR PAST TO RADIOLOGY, SIMILAR FUTURE
Like radiology, pathology relies on image analysis, pattern recognition and identifying deviations from the pattern—elements amenable to AI. Now, clinical pathology relies largely on glass slides and light microscopy, but anything that can be digitized will be digitized. Though FDA clearance for digital pathology has been slow, certain uses have been approved (e.g., immunohistochemistry image analysis). A “whole slide” imaging platform from Philips has just been approved. The trend toward digital pathology will continue, and the US will follow the EU, where CE-IVD mark has allowed clinical platforms since 2014. We anticipate that pathology, like radiology, will move closer to clinical medicine.
RADIOLOGY AND PATHOLOGY MAY COMBINE INTO A NEW SPECIALTY, INFORMATION SPECIALIST
As suggested by Saurabh Jha and Eric Topol, information specialists won’t focus on extracting information from histology and images, but rather manage AI-extracted information and place it in the clinical context of the patient.
I think if you work as a radiologist, you’re like the coyote that’s already over the edge of the cliff but hasn’t looked down…People should stop training radiologists now.
Geoffrey Hinton
Creative Destruction Lab’s Machine Learning and the Market for Intelligence conference, October 2016
COGNITIVE SPECIALTIES WILL CEDE GROUND TO ALGORITHMS
Hematology, endocrinology, nephrology and cardiology all rely on collecting, analyzing and synthesizing data. AI anticipates sepsis before there are observable symptoms, allowing for early and more effective interventions. In hematology, an AI algorithm predicted outcomes for certain treatments in chronic myeloid leukemia. Heart disease, kidney failure and diabetic crises move at a slower pace than sepsis, but likewise rely on data inputs.
PRIMARY CARE DOCTORS’ RESPONSIBILITIES WILL MOVE UPSTREAM
Much of day-to-day primary care is algorithmic and driven by protocols, and can be off-loaded to AI and midlevel providers. Increasingly, primary care physicians will lead midlevel teams, focus on complex cases, and manage triage. However, as triage itself becomes more protocol based, AI will begin to make triage decisions. For all cognitive specialties, including primary care, technological inroads will allow doctors (and midlevels) to concentrate on challenging cases and the human aspects of medicine: effective communication, empathy and ethics.
2016: Sedasys system proven effective, but pulled from market because of anesthesiologist pushback
MANY ASPECTS OF PROCEDURAL MEDICINE WILL BE PROTECTED FROM AUTOMATION
Technology will assist, rather than replace, surgeons and proceduralists. For some specialties, components of p ractice will change. Dermatologists, for example, may not evaluate a lesion’s malignancy—which will be done remotely with cell phone pictures fed through AI—but will still perform the biopsy.
2016: An AI algorithm performed as well as dermatologists in assessing common malignant lesions
INTEREST IN CLINICAL INFORMATICS WILL INTENSIFY
The Clinical Informatics subspecialty was of officially recognized by the American Board of Medical Specialties in 2011. Formal fellowship programs began in 2014 and have grown from one (at Stanford) to 26. The deluge of collected health data, the increasing use of AI and analytics to make sense of the data, and the challenges of applying it to clinical situations (both individually and to a population) mean that the demand for MDs formally trained in clinical informatics will explode. Certification for nonphysicians in clinical informatics will also increase.
-
400 SurgeriesSuccessful use of a closed-loop autonomous robot anesthetist, 2016 clinical trial
THE GEOGRAPHIC MALDISTRIBUTION OF DOCTORS WILL MATTER LESS
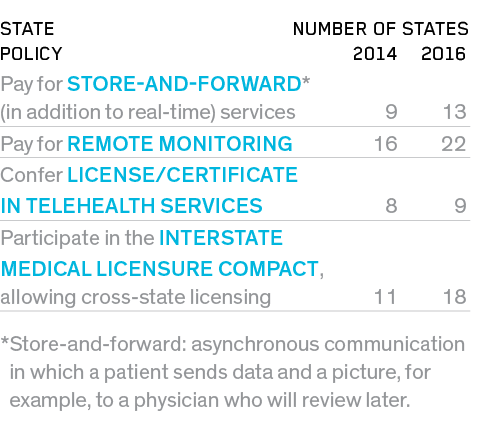
As some policy experts suggest, maybe there’s not an overall shortage of doctors, just a shortage in some places (and an oversupply in others). Washington, DC, has 103 doctors per 100,000 people; Mesa, AZ, has 50. Telehealth, telemedicine and remote monitoring mean that many cognitive physicians will be able to live anywhere. In other words, a doctor living in DC will be able to treat and coordinate care (delivered on the ground by nonphysicians) for a patient in Mesa. However, the regulations governing telehealth—for both reimbursement and licensure—are complex, confusing and often set at the state level. Though political will to advance telehealth appears to be building, the lack of standard policies continues to hinder large-scale adoption.
- 48 states have some form of reimbursement for telehealth in public (Medicaid) programs.
- 31 states and Washington, DC, have private-payer parity laws for telemedicine, up from 18 in 2013.
PROGRESS IN STATE TELEMEDICINE REGULATION
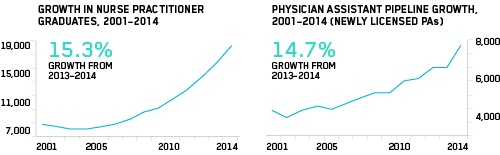
NONPHYSICIAN PROVIDERS WILL GROW IN NUMBER AND IN SCOPE OF PRACTICE, ALLEVIATING ANTICIPATED PHYSICIAN SHORTAGES
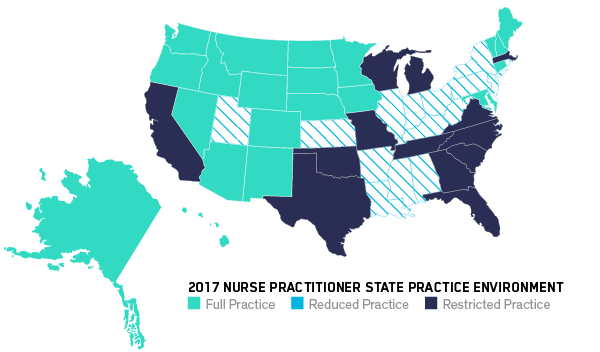
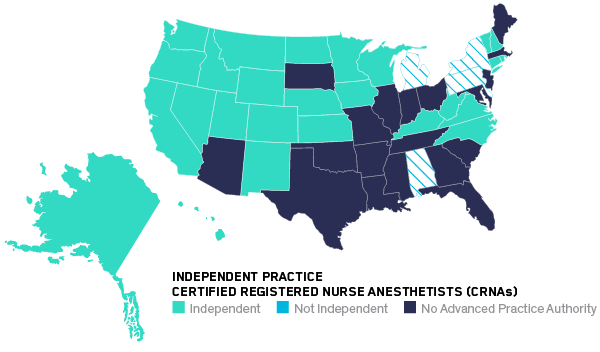
In primary care, nurse practitioners (NPs) and physician assistants (PAs) have been shown to deliver care equal to that of MDs and cost much less. Nurse practitioners have full practice autonomy in 23 states and Washington, DC, up from 20 in 2014. Nurse anesthetists can operate independently (without the supervision of an MD) in 27 states, including Washington, DC, up from 17 in 2014. Even pharmacists are pivoting to clinical care. In California, pharmacists won the authority to prescribe certain medications, such as nicotine replacement and hormonal birth control.

No study has found a difference in the quality of care delivered by nurse anesthetists versus MD anesthetists.
Using midlevels [NPs and PAs] for primary care is very effective [and is] a way forward to tackle the primary care shortage.
Fredric Meyer
dean of Mayo Clinic School of Medicine
THE RELIANCE ON UNLICENSED ASSISTIVE PERSONNEL (UAP) WILL INCREASE
UAP are the nation’s nursing assistants, home health workers and others who provide bedside care and help with patients’ daily activities. Already in hypergrowth, the market for UAP will intensify, driven primarily by demographic trends, e.g., the aging population. Active remote patient monitoring and AI-assisted predictive analytics (engaging the patient before she gets sick) mean that healthcare will move further downstream, from doctor to nonphysician provider to UAP and (finally) to the patient. MOOCs and Khan Academy–type open courses will allow UAP to acquire specific skills for semi-skilled duties.
THOUGH THE RANKS OF UAP WILL SWELL, SOME NONPHYSICIAN HEALTHCARE WORKERS WILL SEE THEIR JOBS CHANGE (OR DISAPPEAR)
At medical centers such as UCSF, Geisinger Health and the University of Pittsburgh,
robots perform orderly duties (delivering lab specimens,surgical supplies, meals, linens, etc.). At UCSF, a robot pharmacist has delivered more than a million prescriptions over five years with 100% accuracy, replacing five pharmacy technicians.
In primary care, nurse practitioners deliver as high quality care and produce as good health outcomes as MDs.