The Doctor’s Assistants Will See You Now
THE GEOGRAPHIC MALDISTRIBUTION OF DOCTORS WILL MATTER LESS
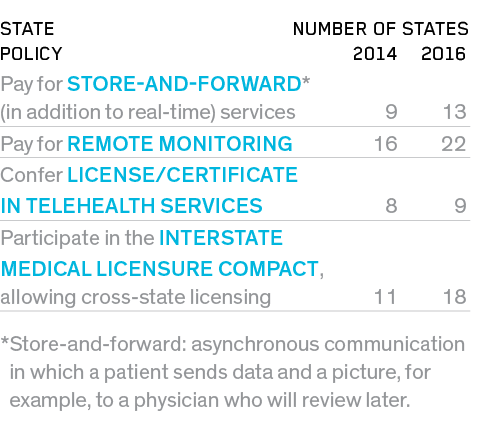
As some policy experts suggest, maybe there’s not an overall shortage of doctors, just a shortage in some places (and an oversupply in others). Washington, DC, has 103 doctors per 100,000 people; Mesa, AZ, has 50. Telehealth, telemedicine and remote monitoring mean that many cognitive physicians will be able to live anywhere. In other words, a doctor living in DC will be able to treat and coordinate care (delivered on the ground by nonphysicians) for a patient in Mesa. However, the regulations governing telehealth—for both reimbursement and licensure—are complex, confusing and often set at the state level. Though political will to advance telehealth appears to be building, the lack of standard policies continues to hinder large-scale adoption.
- 48 states have some form of reimbursement for telehealth in public (Medicaid) programs.
- 31 states and Washington, DC, have private-payer parity laws for telemedicine, up from 18 in 2013.
PROGRESS IN STATE TELEMEDICINE REGULATION
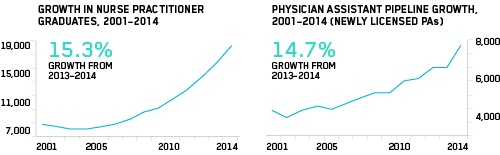
NONPHYSICIAN PROVIDERS WILL GROW IN NUMBER AND IN SCOPE OF PRACTICE, ALLEVIATING ANTICIPATED PHYSICIAN SHORTAGES
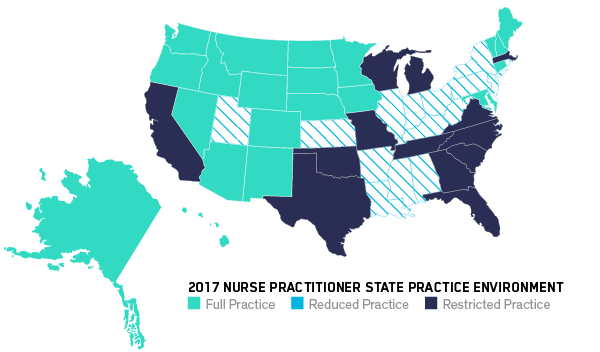
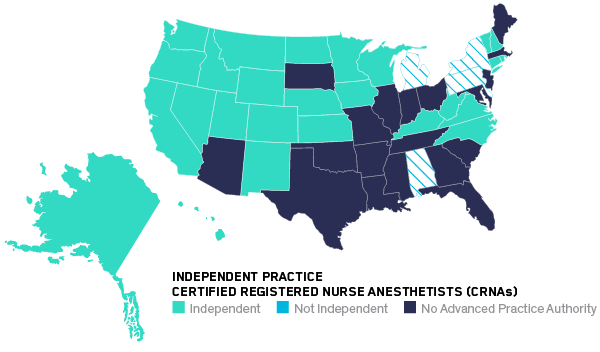
In primary care, nurse practitioners (NPs) and physician assistants (PAs) have been shown to deliver care equal to that of MDs and cost much less. Nurse practitioners have full practice autonomy in 23 states and Washington, DC, up from 20 in 2014. Nurse anesthetists can operate independently (without the supervision of an MD) in 27 states, including Washington, DC, up from 17 in 2014. Even pharmacists are pivoting to clinical care. In California, pharmacists won the authority to prescribe certain medications, such as nicotine replacement and hormonal birth control.

No study has found a difference in the quality of care delivered by nurse anesthetists versus MD anesthetists.
Using midlevels [NPs and PAs] for primary care is very effective [and is] a way forward to tackle the primary care shortage.
Fredric Meyer
dean of Mayo Clinic School of Medicine
THE RELIANCE ON UNLICENSED ASSISTIVE PERSONNEL (UAP) WILL INCREASE
UAP are the nation’s nursing assistants, home health workers and others who provide bedside care and help with patients’ daily activities. Already in hypergrowth, the market for UAP will intensify, driven primarily by demographic trends, e.g., the aging population. Active remote patient monitoring and AI-assisted predictive analytics (engaging the patient before she gets sick) mean that healthcare will move further downstream, from doctor to nonphysician provider to UAP and (finally) to the patient. MOOCs and Khan Academy–type open courses will allow UAP to acquire specific skills for semi-skilled duties.
THOUGH THE RANKS OF UAP WILL SWELL, SOME NONPHYSICIAN HEALTHCARE WORKERS WILL SEE THEIR JOBS CHANGE (OR DISAPPEAR)
At medical centers such as UCSF, Geisinger Health and the University of Pittsburgh,
robots perform orderly duties (delivering lab specimens,surgical supplies, meals, linens, etc.). At UCSF, a robot pharmacist has delivered more than a million prescriptions over five years with 100% accuracy, replacing five pharmacy technicians.
In primary care, nurse practitioners deliver as high quality care and produce as good health outcomes as MDs.