By 2040, a combination of mega-cities, climate change, an increasing global population and high rates of travel will result in the first influenza-based major pandemic of the 21st century. This will galvanize political will and spur development of technology to accelerate vaccine production and distribution.
As the world’s population lives longer, latent disease and disease of the aged or infirm will increase dramatically.
Globally, lifestyle diseases will reach pandemic levels.
NATO-LIKE FIRST RESPONDERS
As global epidemic response shifts away from policy and toward technological innovation and rapid, coordinated first response and delivery, the WHO will become increasingly irrelevant in the initial response stages. During recent global epidemics, for example, NGOs have taken more and more of a role in the first weeks and months because of their legal and social flexibility.
Eventually, a NATO-like organization for global health will need to be created, capable of coordinating basic prophylactic and anticipatory measures. Preparatory drills, coordination of supply chains and rapid intervention agreements could ensure readiness. Aging military or naval equipment, likely from the US or other developed countries, will be repurposed for epidemic-specific stockpiling of resources and people.
Sovereign rights against intervention will muddle international efforts to stem epidemics. The 21st century could see an armed conflict begun over stymied attempts at quarantine during an early-stage epidemic.
DNA SENTINELS TO DETECT OUTBREAKS IN DEVELOPING COUNTRIES
A pandemic or threat of a pandemic will mobilize the placement of “sentinels” in jungle, rural or developing hotspots as well as major destinations and settings for disease transmission like airports, train stations, borders and hospitals. Devices will rapidly detect a fever or sickness behaviors—altered gait, sneezing or coughing—and rapidly sequence ambient DNA, allowing for the detection of viruses or bacteria at international borders.
The Zika virus was detected as early as the 1940s in Africa. A few cases in Asia in the second half of the 20th century preceded its arrival in Brazil, where it then mutated, likely, in the northern jungles before finally spreading to urban populations and rapidly from country to country. Many such other viruses are likely lying dormant in so-called host reservoirs. Sentinels will be required to detect and suppress would-be epidemics in their earliest stages.
We can do the job, if we have the resources.
Dr. Margaret Chan
former Director-General, World Health Organization
-
8.5%Adults with diabetes
-
42%American obesity level by 2030
CLIMATE CHANGE WILL EXPAND DISEASE HOST RANGES
Based on climate change predictions, the host range of many disease-carrying mosquitoes and insects could extend to the US, afflicting poor, rural parts of many Southern and Gulf Coast states.
Changes in local ecologies, water temperature and host and vector availability, upon which many diseases depend, could imbalance microorganism competition, leading to unexpected blooms of disease. Species of Salmonella, for example, increase reproduction as temperatures rise within a range of 7oC–37oC. Increased temperatures may also have unintended benefits—the malaria parasite ceases development above 33oC.
LIFESTYLE DISEASE AVALANCHE
10 million people die of communicable diseases per year, 18% of total worldwide deaths. According to the WHO, diseases linked to lifestyle choices lead to the early deaths of an additional 16 million people per year.
8.5% of adults have diabetes.
Lifestyle diseases like diabetes, which kills 1.5 million per year and contributes to the deaths of another 2 million per year, and obesity, which contributes to the deaths of 2.8 million per year, will reach pandemic status.
By 2030, the CDC predicts that 42% of Americans will be obese and that 11% will be severely obese. Based on 2010 levels, such an increase would add an estimated $549.5 billion to total medical expenses.
Major grocers could begin targeting consumer diets personalized to genomes or offer disincentivization pricing for at-risk individuals, effectively taxing lifestyle disease.
Portable food scanners will allow people to test the composition of their food and track their diet using apps. With a concerted effort, the food industry could work with health technology companies to make poor diet the new smoking: inconvenient, costly and socially unacceptable. The alternative: obesity becomes the new normal, stalling or reversing the overall increase in life expectancy.
The FDA recently approved the first artificial pancreas, and closed-loop (fully automated) versions are in development. Combined with gamification of diet and health, digital contact lenses and implantable or biometric tattoos will help manage chronic conditions like diabetes.
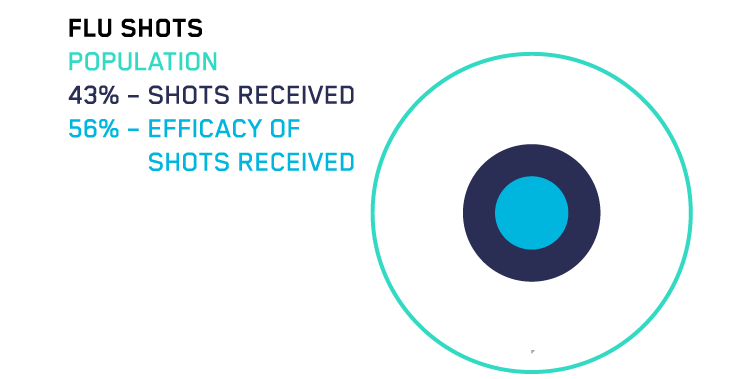
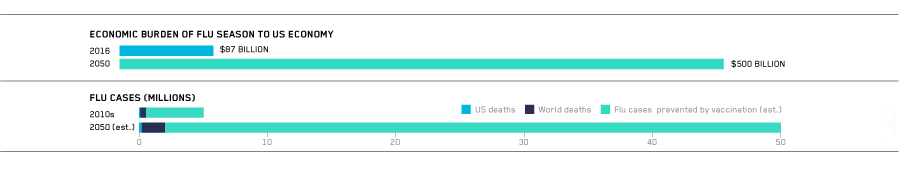
SEASONAL FLU
Only 43% of people get a seasonal flu shot. In a recent year, the CDC reported that only 56% of people who received the vaccine were protected.
Influenza kills half a million people and seriously sickens five million more every year. Influenza was the leading cause of death in the US in 1900 and will be again by 2050 due to an aging population and vaccine ineffectiveness among the elderly.
By 2050, because of an increasingly susceptible and longer-living elderly population, the economic impact of dealing with seasonal flu alone will grow from $87 billion (2016) to $500 billion per year.
We simply need a better vaccine against influenza, one that works better and lasts longer.
Dr. Thomas Frieden
former director, CDC
A MUTATING ENEMY
Mutations in individual nucleotides accumulate in an influenza virus and lead to seasonal vaccine ineffectiveness. Influenza pandemics like those seen in 1957, 1968 and 2009—and like those to come—are due not to small, pointed mutations but instead to re-assortments of the viral genome when two or more viruses combine to create a new subtype. This commonly occurs after passing from animal to animal or animal to human.
VACCINE DEVELOPMENT
The pace of vaccine development will increase steadily as rapid sequencing technology interacts with the printing and on-demand and decentralized manufacturing of proteins. No longer will a few private companies manufacture and distribute vaccines. Instead, federal agencies will develop and send protein “blueprints” to global pharmacies for printing. This will greatly increase the pipeline speed from detection to inoculation and effectively eliminate the infrastructure problem of vaccine distribution. The problem of an individual’s choice to not vaccinate will still remain.
One day, bioelectronic, immune-like cells will be able to hunt, cut up or otherwise target viruses. They will also be programmable. Vaccines will be simple software updates. No shots needed. Today, many major disease-causing viruses are either preventable, treatable or can be managed with chronic care. Vaccine technology is less than half the battle. Access to care remains the biggest hurdle for global treatment.
THE “PENICILLIN MOMENT” IN ANTIVIRAL RESEARCH
There were almost 100 million virus-associated deaths in the 20th century. More than half of all virus-related deaths in the 20th century were due to influenza and its variants.
For a few years, penicillin was a singular “silver bullet” against bacterial diseases. In the future, a combination of surveillance and early outbreak detection, rapid vaccine development and immune system engineering could result in a post-virus world. By the end of the 21st century, viruses will still exist, and people will still die from them, but not in nearly the numbers they did in the 20th century.
HUMAN STRAIN + HIGHLY PATHOGENIC NON-HUMAN STRAIN = HIGHLY PATHOGENIC HUMAN STRAIN
[The greatest risk] to human health comes in the form of antibiotic-resistant bacteria. We live in a bacterial world where we will never be able to stay ahead of the mutation curve. A test of our resilience is how far behind the curve we allow ourselves to fall.
World Economic Forum
DISEASE LATENCY
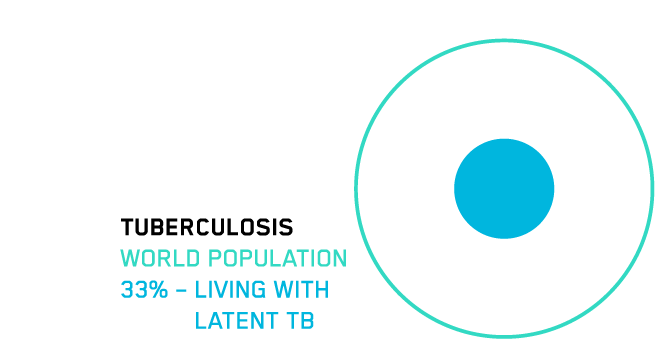
Up to one-third of the world lives with latent tuberculosis infection.
Tuberculosis (TB) is responsible for 1.8 million deaths per year, and both multi-drug resistant (MDR) and extensively drug resistant (XTR) TB are on the rise.
India has the highest burden of TB, a ticking time bomb. Any number of relatively likely immunological challenges—a new HIV-like virus, a low-level radiation event on the Pakistan border—could cause a reoccurrence of TB and multiplicative effect of MDR and XTR TB, which could then spread from India.
MANAGING ANTIBIOTIC RESISTANCE
Antibiotic resistance is projected by some to kill 50 million per year by 2050—about the same as the total number of deaths in 2016 from all causes combined.
This could come at a total economic cost of $100 trillion.
Despite this, there is an almost total collapse of the antibacterial R&D pipeline.
In response to major crises, many dozens of novel antibiotic technologies will be developed, like designer bacteriophages or nano-spike surface coatings.
As of 2016, 40 new antibiotics were in clinical development. However, novel antibiotic development is poorly incentivized—only one in five drugs admitted to Phase 1 trials make it to patients, and in some cases the drugs can be obsolete by the time they finish trials. As market incentives decrease even further for the development of antibiotic drugs, a federal agency will be put in charge of antibiotic technology, stockpiling and development.
Gentlemen, it is the microbes who will have the last word.
Louis Pasteur