For a century, the leading edge of medicine was always invented for rich countries, and slowly trickled down to poor countries. The developing world got the hand-me-downs—everything from medical school training to diagnostic equipment to clinical practices lagged some number of years behind the newest innovations. Modeled on our system, developing-world systems were always playing catch-up, perpetually forced to compromise by the lack of money.
BUT THAT STORY IS CHANGING
Fired up by grants from the Gates Foundation and other NGOs, first-world inventors are now designing new ultra-low-cost products aimed straight for the developing world. Hackathon projects are turning into startups with solutions for third-world medical needs such as malaria, HIV and cervical cancer prevention. At the same time, local innovators in the developing world have been energized to invent their own solutions for low-resource settings. The benefits have been astounding:
-
01Maternal mortality has been cut in half, partly due to widespread distribution of 40-cent medical kits to prevent infections.
-
02Infant mortality has been cut in half.
-
03Cervical cancer can be cut by a third with a simple test using common vinegar to check for lesions.
Much of Africa skipped landlines and went straight to wireless. Africa also leapfrogged branch banking and ATMs, adopting mobile banking and micro- credit earlier than the developed world. In a similar way, much of the underdeveloped world has never seen a hospital, and barely ever seen a doctor. But a radically different, low-cost, leapfrog medical system is emerging. As it improves, we will inevitably ask, “Is there anything they’ve figured out that we should learn from?”
Rich countries can learn a great deal about health and human services from poorer ones… Combining the learning from rich and poor countries can give us new insight on how to improve health.
Lord Nigel Crisp
former CEO, UK National Health Service
OUTFITTING DISTRIBUTED MEDICAL CENTERS ACROSS THE DEVELOPING WORLD IS ABOUT TO BECOME 10x MORE AFFORDABLE
Though considered inferior now, these low-cost technologies will evolve rapidly and improve in quality.
FIRST-WORLD STANDARD OF CARE V.S. 10x AFFORDABILITY (OR MORE)
$2,000Charge for anesthesia | $200Per procedure with anesthesia robot | |
$3,000Blue light phototherapy machine for jaundiced babies | $350Machine from D-Rev which uses LEDs that last 10 times longer than CFL bulbs | |
$3,000–$40,000Ventilators | $300OneBreath ventilator that runs on a 12-volt battery | |
$1,100Vacuum pressure wound therapy kit to speed healing | $3Hand pump developed for disaster relief teams | |
$15,000GE MAC 5500 HD ECG machine | $388GE MAC i ECG machine | |
$20,000Premature infant incubator | $25Embrace infant warmer that’s “recharged” by submerging in hot water | |
$50,000Molecular microscope | $3,500Mobile ultrasound system for midwives, or $500 smartphone attachment | |
$115,0004-D ultrasound systems | $300Butterfly’s ultrasound-on-a-chip smartphone attachment. | |
$1,500,000MRI machines that rely on huge superconducting magnets, so have to be housed in special suites | $50,000Ultra-low-field MRIs, operating at 6.5 millitesla, which use 450x less power | |
The network for a new hospital today is built with 192 strands of fiber and 29,000 Cat 6 drops; TIA-1179 shielded network cable to every workstation. | Mesh wifi connected to urban hubs via 5G |
LAB-ON-A-CHIP DIAGNOSTICS
In many countries, clinics have the drugs to treat a disease but lack the diagnostic tools to screen patients for treatment. For instance, the survival rate of breast cancer patients in low-income countries is half what it is here, due to lack of affordable early diagnostics.
Recent advances in microfabrication and nanofabrication have powered the invention of single-use chip tests that replace traditional laboratory synthesis and chemical analysis. These chips, which can be printed in high volume, come packed with micro-scale pumps, capillary channels and reagents for less than a few dollars per chip. They produce results at the point of care rapidly, and can be used in physicians’ offices, in the field or even at home.
- 274 companies are contributing to the market with their expertise.
- Inkjet printers using nanoparticle ink can produce tests for 1 cent each.
- Dr. Aydogan Ozcan at UCLA has invented a lab-on-a-chip cytometer for $5 to help the 90% of people with HIV who have never been tested for the disease.
CAPABILITIES THUS FAR
-
01
YEAST CELL VIABILITY
-
02
METASTATIC CELL DETECTION
-
03
GOUT DIAGNOSIS
-
04
ENZYME ASSAYS
-
05
TARGETED DNA SEQUENCING
-
06
ANTIMICROBIAL RESISTANCE
-
07
EBOLA
-
08
DENGUE AND YELLOW FEVER
REVERSE INNOVATION
Popularized by Dartmouth professors Vijay Govindarajan and Chris Trimble, the concept of reverse innovation refers to products and methods adopted and perfected first in the developing world before they are spread to the industrialized world. Mobile banking and micro-finance were the first noted examples, but now there’s a deluge of innovations: biomass gasification power plants, small steam turbines, battery-powered home refrigerators, infotainment systems for motorbikes, etc. Doctors in Alabama running an AIDS clinic turned to Zambia to learn how to make sure patients attend follow-up appointments.
CLASSIC DISRUPTION THEORY
Clayton Christensen’s disruption theory describes how market leaders are knocked off their pedestals not by innovation at the high end, but from underneath. Entrants gain a foothold by delivering to low-end markets over-looked by incumbents. They are considered inferior by most of the market, but with constant improvement reach quality standards that serve the middle market.
LEARNING FROM INDIA
In India, the average patient pays 65% of their costs out of pocket, on extremely limited resources. Hospitals there have learned to treat problems of the eyes, heart and kidneys, provide maternity care and orthopedic medicine, and treat cancer for less than 10% of US costs.
Microinsurance
With premiums as low as $5 a year, microinsurance pulls rural communities into health networks, offering tele-medicine, catastrophic coverage for birthing complications and immunizations. Cellular service providers even offer free health microinsurance for customers who buy monthly minutes.
50-cent E-Consultations
Max Healthcare in India extends its hub- and-spoke network into 400 Punjab villages by setting up telemedicine kiosks at safe drinking water access hubs.
$1,500 Cardiac Bypass Surgery
Cost in US: $144,000 Cost in India: $1,500*
How they do it:
- High-volume specialization allows a grafting surgeon to operate on 5–6 patients per hour. Chest opening, vein harvesting and suturing are performed by junior doctors.
- Sterilization and reuse of surgical tools
- Manufacturing of stents for 1/10th the cost
*Mortality and infection rates are comparable to good American hospitals.
$41 Cataract Surgery
Aravind Eye Care, inspired by McDonald’s high-volume service, has performed 4 million operations. Paying patients, who are charged $41 to $125 depending on the surgery, subsidize free surgery for the poor. All surgeons rotate between paying and free wards. Intraocular lenses are manufactured for only $2.
THE GLOBAL MIDDLE CLASS
In a decade, the booming Asian middle class will be 6x the size of the American middle class. While the wealthy will buy Western medical care, the new middle class will get its medical care through systems imported from the developing world, including microinsurance, e-consultation services, assembly-line surgery and birthing care.
Life science is easier to model on a computer than in wet form. The more medicine gets digitized and becomes an information product, the more it will follow Moore’s law.
Steve Jurvetson
venture capitalist
VALUE-BASED CARE
The lifespan gap in the US between the rich and the poor has doubled since the 1970s—not due to quality of care, but to care accessibility. Rewarded by new value-based pricing, community health centers will look abroad for wisdom and methods. In New York State, Medicaid is migrating to value-based care by 2020. The Greater Buffalo United Accountable Healthcare Network is running an 8,000-patient pilot program through a network of community-based private practices. Community health workers call and visit chronic-care patients in their homes. Adopting the customer-service methodologies of retail, a new holistic clinic offers a gym and nutrition kitchen on the first floor, primary care on the second floor and specialists on the third floor.
MEDICAL TOURISM
Medical tourism started with patients coming to America to get the best treatment. In the last decade, far more patients have been going the other direction, for everything from heart valve replacements to fertility treatments to addiction recovery. More than 1 million Americans a year cross borders for treatment. These patients return as de facto ambassadors testifying to the quality of low-cost care.
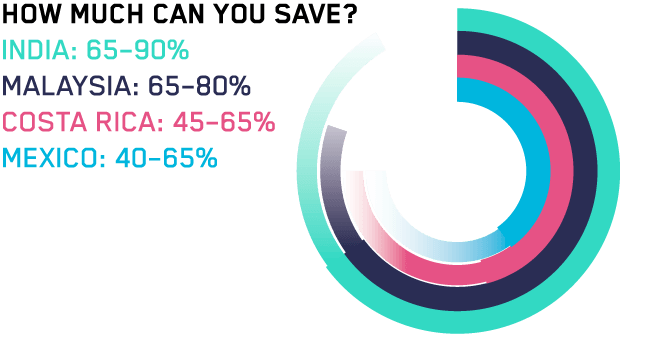
Health City Cayman Islands, founded by renowned Bangalore heart surgeon Devi Shetty, offers heart surgery, hip replacement and neurosurgery for 40% of US prices, just a two-hour flight from the Atlantic coast.
CUBA EXPORTS
Isolated from the rest of the world, Cuba invested heavily in biotechnology and public health, developing the capacity to cheaply produce 70% of their pharmaceuticals. 30,000 Cuban medical staff are working in over 60 countries around the world. High rates of lung cancer led to the invention of CIMAvax, a vaccine used for both prevention and post-radiation maintenance. The Roswell Park Cancer Institute is bringing CIMAvax to the American market.