Buried in paperwork, snarled in endless technology turnover, hemmed in by increased performance monitoring and challenged by a new breed of empowered (and often ill-informed) patients, morale among doctors is at the lowest levels ever recorded.
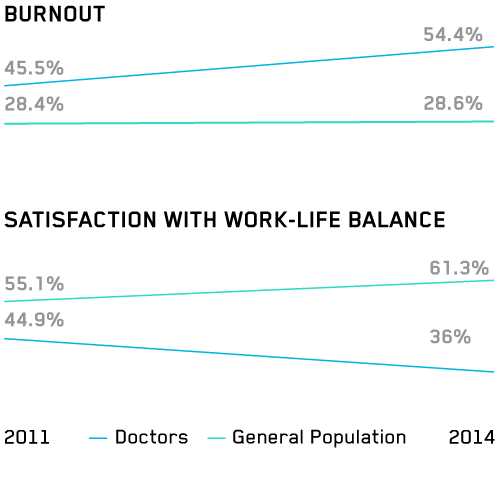
Over half of physicians are burned out and/or dissatisfied with their work-life balance, which compares unfavorably to the general employed population. More than 60% of doctors are somewhat or very pessimistic about the future of medicine, and over half of doctors would not recommend a career in medicine to a young person, with some surveys going as high as 90%. A survey of doctors and nurse practitioners showed:
THE TOP 5 MOST BURNED OUT SPECIALTIES
- EMERGENCY MEDICINE (>70%)
- UROLOGY (63.6%)
- PHYSICAL MEDICINE AND REHABILITATION (63.3%)
- FAMILY MEDICINE (63%)
- RADIOLOGY (61.4%)
Nine specialties showed a >10% increase in burnout 2014 over 2011.
BURNOUT
CAUSES OF BURNOUT
- Loss of autonomy and control over work
- Too many bureaucratic tasks
- Too many patients
- Feeling like “a cog in a wheel”
- Increased performance measures (quality, cost, patient satisfaction)
- Increased complexity of medical care
- Technological fatigue, especially EHRs
- Changes in the doctor-patient relationship (shift from “patient” to “healthcare consumer”), i.e., difficult patients
Maintenance of certification (MOC) is also a driver of physician dissatisfaction. MOC is a recertification program that allows doctors to maintain specialty board status and consists of completing training and evaluative modules, and taking an exam. Doctors complain that it is too burdensome: expensive and time consuming. Internists will spend an average of $23,607 each in MOC costs over 10 years. The cumulative cost of MOC to the healthcare system is estimated to be $5.7 billion over 10 years.
SYMPTOMS OF BURNOUT
- Emotional exhaustion
- Increased depersonalization
- Decreased sense of personal accomplishment
- Depression
- Suicidal ideation
CONSEQUENCES OF BURNOUT
- Early retirement, scaling back clinical duties
- Decreased patient safety
- Decreased quality of care
- Increased healthcare costs
- More testing and referrals
- Greater malpractice risk
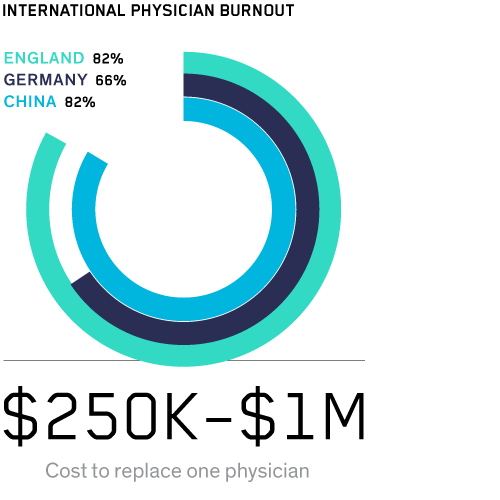
Physician burnout doesn’t just affect doctors. It affects all of us. Burned out doctors make more mistakes and appear to deliver lower quality of care. Beyond patient care and doctor well-being, burnout impacts the bottom line. Replacing a physician who retires early or leaves medicine to pursue other career opportunities costs between $250K and $1M.
AND PHYSICIAN BURNOUT ISN’T JUST A US PHENOMENON
82% of physicians in England experience mental illness. In Germany, 66% of physicians report some degree of burnout. In China, it’s 82%.
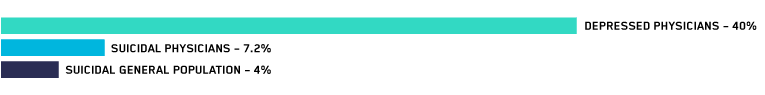
Physician suicide is estimated to be 400 annually, one of the highest rates among all professions. Advocates maintain that physician suicide is under- reported, hushed up, masked. Physician deaths from “accidental overdoses” may actually be suicide, since doctors are unlikely to overdose on medications.
If I wanted to work on an assembly line, I didn’t need to go to medical school. Nothing will change because we are completely expendable.
Physician comments
to “Physician Burnout Is a Public Health Crisis: A Message to Our Fellow Health Care CEOs,” in Health Affairs, 2017
40% of US physicians screened positive for depression. 7.2% had thoughts of killing themselves in the previous 12 months, compared with 4.0% for the general population. And doctors don’t just think about suicide more than the general public—they actually do it more. They’re better at suicide. Greater knowledge and access to lethal methods mean physician completion of suicide is higher than that of the general public, 1.4–2.3×. Female completion is even higher: 2.5–4× that of the general public.
400 / year
Estimated Doctor Suicides
-
American Doctors Are Killing Themselves and No One Is Talking About It
The Daily Beast, March 2015
-
Why Doctors Are Sick of Their Profession
The Wall Street Journal, May 2016
-
The Hidden Epidemic of Doctor Suicides
Fast Company, February 2016
-
The Story Behind Epidemic Doctor Burnout and Suicide Statistics
Forbes, January 2016
A 2016 AMA summit described burnout as a matter of “absolute urgency.” Healthcare leaders have publicly pledged to systematically track and measure physician well-being. The AMA, Stanford and the Mayo Clinic are developing a national consortium on physician wellness.
ZERO PAPERWORK, EFFORTLESS DATA CAPTURE
Making doctors’ lives easier is a booming business. The healthcare AI sector is growing 50% a year, and is expected to top $10 billion in 2023. Some early standouts:
-
AUGMEDIX
uses AR headsets to stream doctor-patient interactions to remote scribes, reducing documentation time by 80% and saving doctors up to three hours a day.
-
HEALTHTENSOR
reviews data in patients’ medical records to help doctors instantly pick the correct ICD codes for diagnoses and procedures— out of 68,000 possible choices.
-
CLOUDMEDX
combs through patients’ medical histories and clinical databases to give doctors real-time risk assessment and decision support during patient visits.
WAYS TO IMPROVE PHYSICIAN MORALE
-
Optimize physician support in the practice environment
-
Train healthcare leaders to foster physician engagement
-
Improve physician career fit
-
Foster a sense of community and flexibility, thereby giving physicians more control
-
Create programs for physician well-being
Improvement will accelerate as physician wellness is tied to existing metrics: patient satisfaction, quality of care, productivity. In addition to more traditional cost centers (supplies, capital equipment), healthcare organizations will account for the true price of physician burnout. Standout organizations will highlight physician satisfaction to boost recruiting.
Complicated EHR systems are the bane of physicians’ workdays. Most doctors spend almost twice as much time wrestling with EHRs and other desk work as they spend with patients. In order to retain physicians, hospital systems will pressure existing EHR vendors to improve user interfaces— or they will upgrade to new, improved EHR systems.
In the near term, hospitals and practices will unburden physicians of clerical/administrative duties via medical scribes, who follow doctors through their clinical rounds, taking notes and completing data-entry tasks. Studies show that scribes have a positive impact on both physician satisfaction and productivity. By 2020, the number of medical scribes helping doctors is projected to jump to 100,000, a 5× increase from 2014.
Doctors’ experience in the workplace will improve even more dramatically through the 2020s, as automated data collection and AI-powered decision support unburden them from routine tasks, streamline complex processes and reduce the stress of sifting through patient data to find needles in medical record haystacks.